There have been many mechanisms proposed linking the jaw joint and its muscles (TMJ) and neck (C/S) postural problems. Sitwell a dentist in 1927 was one of the first to document the interrelationship between occlusion and posture. More recently Makofsky proposed the ‘sliding cranium theory’ (1989). In this essay I would like to discuss the anatomical and functional mechanisms that account for this commonly encountered relationship of jaw and neck pain.
The term craniomandibular dysfunction (CMD) is being used to describe the complex condition involving abnormal jaw mechanics incorporating dysfunction of the masticatory muscles and the temporomandibular joint.
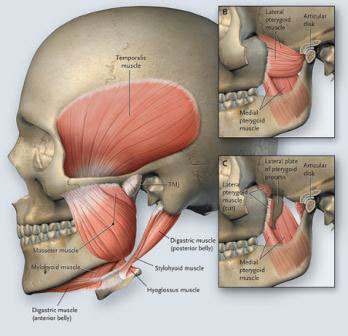
These muscles include the Masseter which action is to elevate, close and retrude the mandible. Overstress of this muscle is common and may be linked to psychological stress, occlusal disharmony or trauma.
Temporalis acts to close the jaw, retrude the mandible and unilateral deviation to that side. Tension in this muscle has the same causes as the Masseter also including mouth breathing and excessive gum chewing (Travell and Simon). The Lateral Pterygoid opens and protrudes the jaw bilaterally and deviates it unilaterally to the opposite side. The superior division of this muscle exerts traction on the disc and the inferior division assists in condylar translation essential for full mouth opening.
Therefore this muscle is directly related to malocclusion and” clicky jaw”. The Medial Pterygoid acts to elevate the mandible and laterally deviate it to the opposite side. Symptoms arise from opening the mouth chewing, clenching and swallowing. The Digastric muscle may lift the hyoid bone, open and retrude the mandible.
Patients presenting with CMD often have limited range of the jaw joint (55mm of mouth opening and 12mm lateral deviation is considered normal – measured with a therabite). They may have clicking and grinding and often have symptoms such as headache, facial pain, deafness, tinnitus, fullness in the ear, vertigo and throat pain. These local symptoms almost always accompany a forward head posture and chronic upper cervical extension.
A relationship between CMD and head position described by Makofsky proposes that as the cranium tilts backwards the occiput is translated anteriorly on the atlas causing a simultaneous shift of the whole maxillary dentition in relation to the mandible. This is then forced anteriorly to obtain occlusal support. This will affect the muscular balance of the neck (SCM, scalenes, sub occipitals, traps etc.) and the TMJ (Pterygoid, Temporalis, Masseter and hyoid muscles).This complex relationship can move in an ascending or descending manner. Clinically it seems vital to treat and manage the jaw and neck pain as interdependent entities.
There are three main theories that contribute to the development of CMD which overlap significantly but include Muscular, Psychological and Malocclusion theory. Stress creates bruxism particularly at night. Muscles become tight and thicker, the jaw alignment deteriorates .The cranium slides and the upper cervical spine heads into permanent extension. I can’t see the chicken or the egg in this pattern but the meat in the CMD sandwich is sure to be the airway and breathing patterns.
I believe the breathing pattern is of vital importance in understanding the close relationship between the jaw and the neck. Let me describe a couple of common presentations.
Desk bound Dave works long hours at his desk in a fairly stressful role. He catches the bus to work and often eats his lunch at his desk. Dave drinks two coffees a day.
Let’s consider the physiology. Dave spends too much time sitting, over time his hip flexors get shorter and shorter. Dave’s pelvic diaphragm balance is lost and his belly breaths become shallower. Add some caffeine and some deadlines and Dave recruits an upper respiratory breathing pattern and therefore uses Pecs and his scalenes to help inspiration. The Pecs contribute to increasing his thoracic kyphosis and the scalenes then draw the neck forward into a larger cervical lordosis. Tension is experienced in the sub occipitals and the sliding cranium theory is in full flight. If the first symptom of this pattern is picked up by the dentist as a malocclusion then I’m not sure if Dave would benefit from a night splint? This would represent an ascending example of CMD.
Mouth breather Molly is only 21 but has experienced headaches for years.
Molly broke her nose when she was 15 and since then hasn’t been able to take a full breath through her nose. During the day she tends to breathe with her mouth open, at night she sleeps on her side with her neck in extension and with resting tension in her Pterygoid muscles in an attempt to maintain an airway when she sleeps. Not surprisingly Molly usually always wakes with her headache. Molly has a rather large range of unsuccessful therapeutic pillows. Molly is typical of a descending pattern of CMD.
The treatment plans for these two clients would be vastly different but also share a common thread of pain, postural decline and muscle imbalance.
Hopefully in this essay I have highlighted the mechanisms for developing jaw and neck pain and how intimately they are related in the syndrome of CMD.